Technology is rapidly changing many areas of life, including healthcare. This is an important topic because using these tools can greatly improve the lives of elderly people, especially those in rural areas who may not have easy access to healthcare. With more elderly people living in rural areas, access to adequate healthcare becomes a big concern. This group often has unique healthcare needs because of chronic illnesses and other health issues. Servicing these needs is made harder because of their location, which can be far from needed services. Regular in-person care can be difficult to provide, which means there's a strong need for online health tools to provide remote healthcare services. Online health—using a broad term that refers to any health service or information provided online—can be a great solution. It lets us regularly track, consult, and treat elderly individuals.
Learning the Fundamentals of eHealth Tools
eHealth tools, which integrate technology into healthcare, took a significant leap in the late 1950s with the invention of medical machinery like heart-lung machines. Teaching healthcare professionals to effectively use these tools has become an essential part of medical education only recently. Until the 1990s, medical training was focused on theoretical learning and manually operated equipment.
The boom in digital technology, especially the internet, in the late '90s marked the shift towards a more technologically advanced healthcare system. With computers and the internet becoming fundamental tools in healthcare settings, eHealth literacy became vital. Consequently, educational institutions began incorporating eHealth curriculum into their programs. The early 2000s witnessed the rise of web-based training resources, simulations, and virtual reality tools in medical education. These changes led to significant improvements in the ways professionals are trained and patients are treated.
Understanding the Basics of eHealth Tools
These tools include things like electronic health records, telemedicine, health apps on mobile phones, and wearable technology. They can greatly help older patients in rural areas get the health services they need, as these patients often find it hard to get to a clinic or hospital. Use telemedicine to diagnose, treat, and check up on patients from a distance.
Using electronic health records makes keeping track of a patient's health easy, which is extra useful for older patients who may have multiple health issues. Mobile health apps and wearable devices can help prevent health problems from getting worse by recording important signs, reminding patients to take their medicine, or reminding them to be more active, reducing the need for them to go to the hospital.
Exploring Key Features and Functions of eHealth Tools
They include telemedicine, remote tracking, electronic health records (EHR), and health apps for older people in rural areas. Use these tools to overcome distance barriers in healthcare. Telemedicine is one of them, and it's crucial because it offers online doctor visits, saving both time and money. Remote monitoring is another important feature that helps to keep a close eye on patients’ health and offer personal care. EHRs make it easier for both patients and doctors to access medical information, leading to better diagnosis and treatment. Health apps designed for this group have a lot of promise for self-care. They can help to raise awareness, give advice, and remind users about medications.
The Potential of eHealth Tools in Addressing Rural Geriatric Healthcare Issues
These tools can improve access to healthcare. They help overcome remote location issues, transportation problems, and multiple health conditions due to old age. Telehealth provides immediate health services by connecting healthcare professionals and elder patients in their homes. It skips travel and is excellent for those with movement limits. Use it for regular health checkups, diagnosing symptoms, or urgent medical advice. It can even introduce you to specialists not available in rural areas.
Electronic health records coordinate treatment for the elderly dealing with multiple health issues. These digital records allow healthcare providers to share the patient's whole health history, ensuring accurate and consistent care. Use them for remote patient surveillance to ensure prompt action for unusual health issues. Mobile health applications help elderly patients actively manage their health.
Examples of Successful eHealth Implementations in Rural Healthcare
It uses technology to bring healthcare services to people in remote places. Take, for example, the telemedicine initiative in rural Alaska. This program offers remote consultations to elderly people. Elderly patients can talk to healthcare professionals using video calls, eliminating the need for travel. This convenient method has improved the treatment of chronic diseases and emergency response tactics, which in turn has improved the quality of life for the elderly in these areas.
In rural Australia, a community healthcare program uses digital technology in a similar way. It links central health monitors with digital devices like phones and tablets. This allows elderly patients to track their physical activity, record important health readings like blood pressure and glucose levels, and share this information with their healthcare teams. As a result, disease management has improved greatly, and the overall health of elderly patients has been enhanced. eHealth has also been successfully used in rural South Africa in a program called 'MomConnect.' This initiative sends key health information to pregnant women via essay messages.
Designing eHealth Solutions for Geriatric Patients: Considerations and Requirements
Older patients usually deal with ongoing health issues, less mobility, and certain mental health problems. So, it's crucial to make the technology easy to use to promote its use. When thinking about country areas, online health services need to address problems with internet connection, lack of technical skills, and lack of immediate help. To beat these issues, strong, simple-to-use interfaces with clear instructions are needed for the old living in these regions. All complicated tech language should be avoided, and features like essay size, screen light level, and sound quality should be modified to suit possible sensory problems.
Specific eHealth devices are vital in country areas for watching health information in real time and giving necessary medical services online. These eHealth devices can guarantee that vital medical data is available, and health checks or meetings can be done from a distance or arranged as per their convenience. Internet lessons for the old or their caregivers could be a one-time payment to improve the use of these tools. It's vital to concentrate on making systems that are suitable for a wide variety of health issues common in older people.
Educating Rural Geriatric Patients about eHealth Services: Strategies and Methods
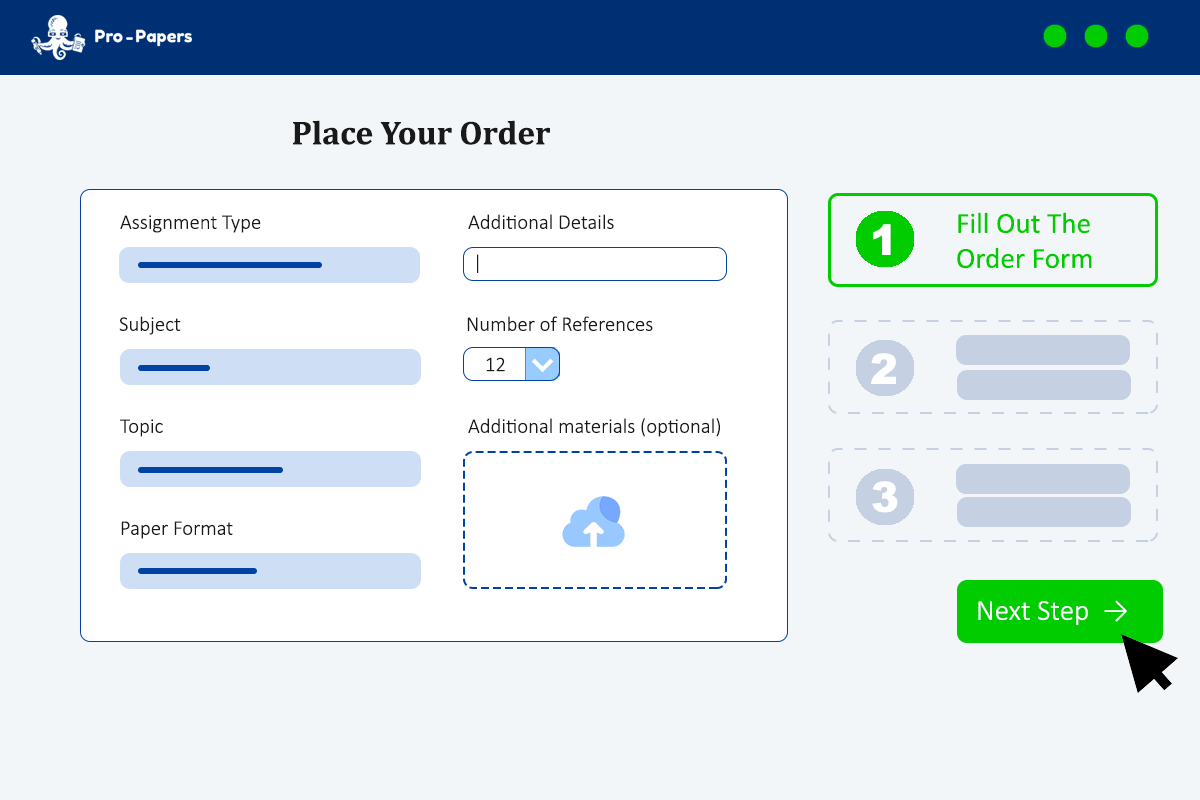
This is because these services can make health care better and easier to access. eHealth includes digital tools like online doctor visits, electronic health records, and wearable devices for monitoring health signs. One good way to teach these adults is to use simple and user-friendly materials. Given that older adults might find technology tough, it's important that these tools are easy to understand. Use simple graphics, booklets with step-by-step instructions, and clearly spoken video tutorials to teach them.
Incorporate technology learning in their regular doctor visits. This can be another effective method. Doctors or healthcare professionals can show the patients how to use the tools, allowing them to try it themselves. This could involve simple tasks like booking doctor appointments online, viewing their test results, or checking their own health status. Another step is to build support networks. This could include family, caretakers, or volunteers who understand how to use eHealth tools. These networks can continuously help and strengthen learning. Community-based training programs can also be really helpful.
Challenges and Solutions in Implementing eHealth for Geriatric Patients in Rural Areas
The main issue is the 'digital divide.' Many older patients struggle to use eHealth tools because they're not used to digital devices or are afraid of them. Also, rural areas often have poor or unreliable internet, making these tools hard to use. Another problem is that rural areas usually have less access to resources. There are fewer healthcare facilities and professionals, making eHealth hard to manage and monitor.
Also, rural patients often have limited money, making the cost of technology a barrier. To fix these issues, train and support older patients in using eHealth tools. Simplify eHealth interfaces and give older patients thorough training. Focus training on using the tools, finding health information, and talking effectively with doctors. Address internet problems by pushing for better infrastructure or using offline technologies that save data until there's a connection.
Solve financial issues by covering some of the costs of eHealth tools or create cheaper options for these patients. You could also partner with tech companies to offer devices at reduced prices. Make sure to design eHealth tools with the elderly in mind, taking their needs, abilities, and preferences into account.
Bringing it All Together
Through internet technologies, we can provide remote consultations, monitoring, and management of health conditions, helping to overcome the challenges of distance and limited access to health services. But we must also work hard to improve computer skills among these people and enhance internet services in their areas. It is crucial to fully adopt this digital healthcare revolution. It's not only about introducing new ways of doing things but also ensuring everyone has equal access to health services. We should include rural older people in eHealth programs.