As we moved into the 20th century, this dynamic began to shift dramatically towards a more patient-centered approach. This change was driven by several factors including increased democratization of knowledge facilitated by advances in education and technology, greater public awareness of health issues, and a growing emphasis on individual rights and autonomy. The rise of the bioethics movement in the 1960s and 1970s further championed this shift, highlighting concepts such as informed consent and respect for patient autonomy. Consequently, communication between doctors and patients started to become more bidirectional, with an emphasis on dialogue rather than dictation. Patients became more empowered to ask questions, express preferences, and actively participate in decision-making about their treatment options. This era also saw the introduction of shared decision-making models, recognizing that both parties bring valuable perspectives to the conversation – doctors contribute their clinical expertise while patients share their personal values and preferences regarding their care. This evolution reflects a broader cultural shift towards valuing individual autonomy and collaborative relationships in healthcare settings.
The Impact of Technology on Medical Conversations
While technology has undoubtedly enhanced many aspects of doctor-patient communication, it also presents new challenges. The reliance on electronic communication can sometimes lead to a depersonalization of interactions, where the subtleties of face-to-face communication are lost. The digital divide remains a significant issue; disparities in access to technology based on socioeconomic status, age, or geographic location can exacerbate inequities in healthcare access and quality. The overwhelming amount of health information available online can lead to misinformation and increased anxiety among patients, complicating medical conversations. Thus, as we navigate this digital era, it becomes crucial for healthcare professionals to strike a balance between leveraging technology to improve medical communication and maintaining the personal touch that is fundamental to building trust and rapport with patients.
Language and Power Dynamics in Healthcare Settings
Efforts to democratize communication in healthcare have emphasized the importance of plain language and shared decision-making. By consciously adjusting their language to be more inclusive and accessible, healthcare professionals can bridge the knowledge gap, fostering a more equitable interaction where patients feel valued and heard. This shift not only empowers patients but also encourages a more collaborative relationship, enhancing patient satisfaction, adherence to treatment plans, and overall health outcomes. Recognizing the diverse linguistic and cultural backgrounds of patients is crucial in tailoring communication strategies effectively. Language concordance and cultural competence training for healthcare providers have emerged as key factors in addressing health disparities and improving the quality of care for all patients. Through these efforts, the dynamic within healthcare settings evolves towards a more balanced power distribution, enhancing both the efficacy of medical conversations and the patient experience.
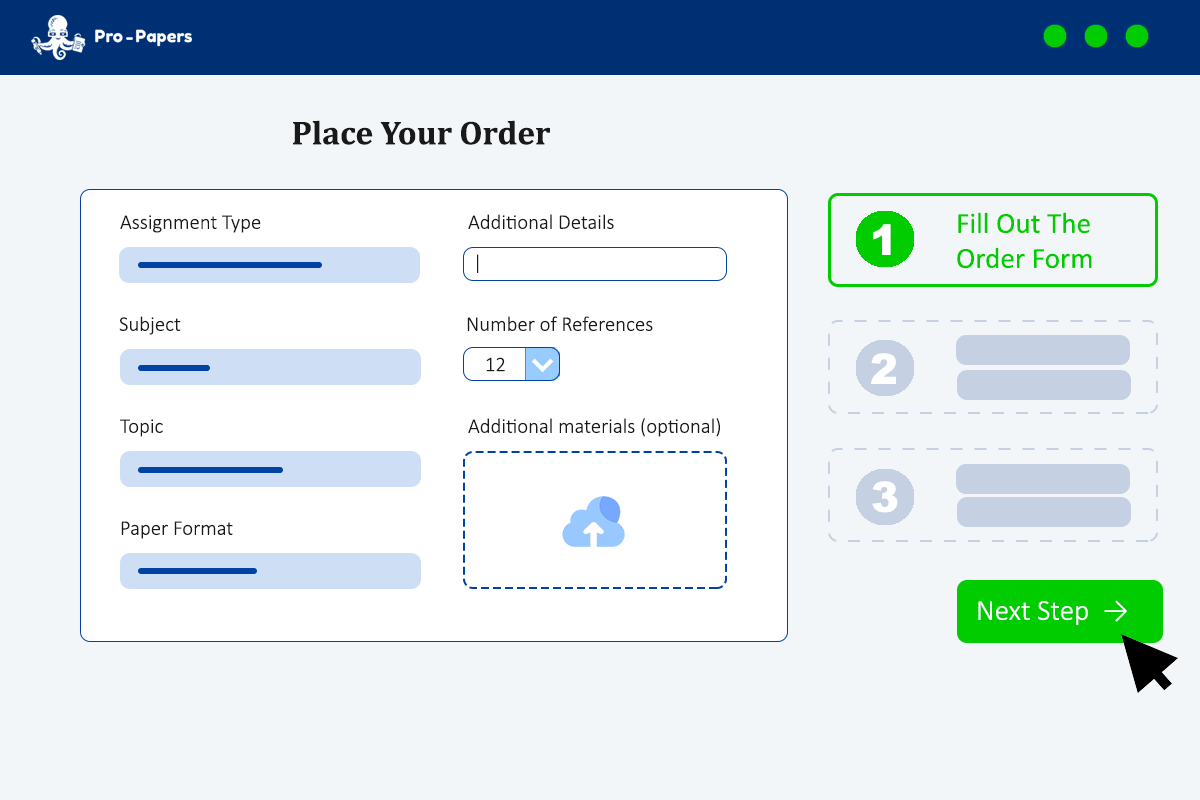
Strategies for Improving Patient Understanding and Engagement
Personalized care plans that take into account a patient's unique circumstances, preferences, and values are becoming more common. This individualized approach promotes a stronger partnership between the patient and healthcare provider. By involving patients in the creation of their care plan, healthcare professionals can ensure that recommended treatments align with patients' life goals and preferences, thereby increasing satisfaction and adherence. Leveraging technology such as patient portals allows for ongoing communication outside of appointments, giving patients direct access to their health information and a convenient way to ask questions or express concerns. Through these multifaceted strategies, the healthcare industry is making significant strides towards enhancing patient understanding, engagement, and ultimately, outcomes in the medical setting.
The Role of Cultural Competence in Doctor-Patient Interactions
Cultural competence extends beyond individual patient interactions to inform broader health policy and practice. Health systems that prioritize cultural competence training for their staff can address systemic biases and improve health outcomes across diverse patient groups. This approach involves not only language translation services but also the integration of cultural beliefs into care planning and decision-making processes. By doing so, healthcare providers can mitigate misunderstandings and potential conflicts, ensuring that all patients feel respected, understood, and cared for. The role of cultural competence in doctor-patient interactions is thus pivotal; it not only facilitates clearer communication but also fosters an inclusive environment where every patient’s health needs are met with sensitivity and respect, ultimately contributing to more equitable healthcare delivery.
Ethical Considerations in Medical Communication
Equity in healthcare communication also emerges as a significant ethical issue. The move towards a more inclusive approach in medical conversations aims to address historical imbalances where certain groups may have been marginalized or not given full consideration due to language barriers, cultural differences, or disabilities. Ensuring equitable access to comprehensible and culturally sensitive information is essential for upholding the ethical principles of justice and beneficence in healthcare. This involves not only adapting communication methods and materials to meet diverse needs but also actively working to dismantle systemic barriers that impede equal participation in healthcare dialogues. By prioritizing these ethical considerations, healthcare providers can foster more respectful, understanding, and effective interactions with their patients, ultimately contributing to better health outcomes and a more just healthcare system.